Behavior Changed, Yes, But Only After COVID Was At Doorstep

The new COVID-19 is an extremely contagious virus (having about three times the transmission rate of the flu), and its spread depends on social contact. For an individual living a normal life, the probability of infection is extremely high (as individuals exhibiting no symptoms tend to go untested). If a sizeable share of the population becomes infected, not only can it directly deteriorate individuals’ well-being, but given the capacity constraints of our health systems, it can indirectly disturb all life-and-death health care activities. Both situations can be fatal or have serious health consequences.
Nonetheless, what is unique about COVID-19 is that, unlike other more common viruses, we know very little about it (the World Health Organization has just started to follow everything published on the virus). This means that there is still significant scientific uncertainty on its effects. Scientists disagree on their findings, and different countries have implemented different preventive solutions to the risks posed by the pandemic. This scenario breeds information scams and false stories, all leading to an alarmist behavior.
When the objective information about the risks of COVID-19 is still unknown, individuals exhibit what behavioral economics calls ‘ambiguity aversion,’ namely the dread of ‘unknown uncertainty’ in evaluating health risks. Although the risks of COVID-19 are small for a majority, for about 20 percent of the population it can have serious consequences, and even be fatal for about 2 percent.
How are scares formed?
Given that most of us do not have enough technical knowledge to form rational expectations about the effect of COVID-19, it is only natural to anchor our perceptions on priors using analogical reasoning. That is, we compare COVID-19 to other similar risks in our memories. However, when it comes to COVID-19, it is hard to find comparable outbreaks. One can compare it to a milder epidemic such as SARS, the H1N1 pandemic or take a more catastrophist perspective and use the 1918 Spanish flu. However, even when making those comparisons, these examples differ in their transmission, interventions and characteristics.

When analogical decision-making fails, a common reaction is to follow some form of social learning, whereby individuals observe what others in their environment do, or how celebrities and other role models behave, and adjust their expectations accordingly. Evidence has consistently shown that health behavior is influenced by how one’s social network behaves and perceives the risk (Scherer & Cho, 2003). This can explain the formation of alarmist decisions and hysterical reactions of different kinds.
Most of us need a narrative to frame and make sense of our actions. However, when it comes to the COVID-19, there is no official narrative. Public authorities in many countries have failed to reassure the population that they have control of the situation. In the meantime, the numbers of infected people and casualties rise day by day, given that popular narratives become extremely sensitive to information primes or stimuli. Alarmist decisions can arise when worst-case scenarios are provided with too much credibility, or when a risk is over-advertised (Viscusi, 1997). Individuals who rely greatly on the media for information are particularly subject to risk overamplification. In some countries, however, the media can play a role in the slow behavioral reaction to COVID-19. An example in the United States is Fox News’s Sean Hannity insinuating that the coronavirus could be a hoax to bludgeon President Donald Trump. The tendency of minimizing risks and delaying reaction is also seen in Brazil, where President Jair Bolsonaro has said that the COVID-19 crisis was hysteria, comparing the coronavirus to a simple flu.
Risk proximity as an explanation
Geographic proximity can explain the slow reaction of some countries to the risks posed by COVID-19. Research shows that risk perceptions about an adverse event are influenced by proximity to risk (Fischhoff et al., 2003). In a previous study, some LSE colleagues and I show that the risk perceptions and behaviors after the avian influenza (H5N1) virus, which hit Europe in late 2005 and early 2006, was related to the proximity to risks. More specifically, we show that if there were human cases of the H5N1 virus in or bordering their country of residence, people were likely to change their consumption behaviors regardless of the level of their knowledge.
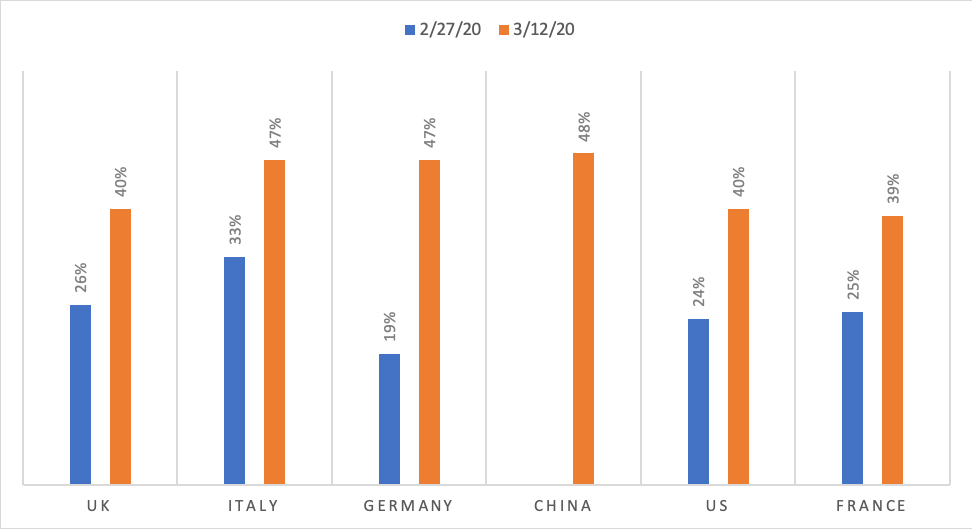
So far, a similar conclusion can be reached once we look at the data from individual reactions to COVID-19. The figure below indicates that, in most European countries, with the exception of Italy, the share of individuals that thought that someone close to them is likely to be infected increased dramatically during the last week of February when the infection rate in Italy was already escalating, but not before.
How likely or unlikely do you think someone close to you will be infected by the coronavirus?
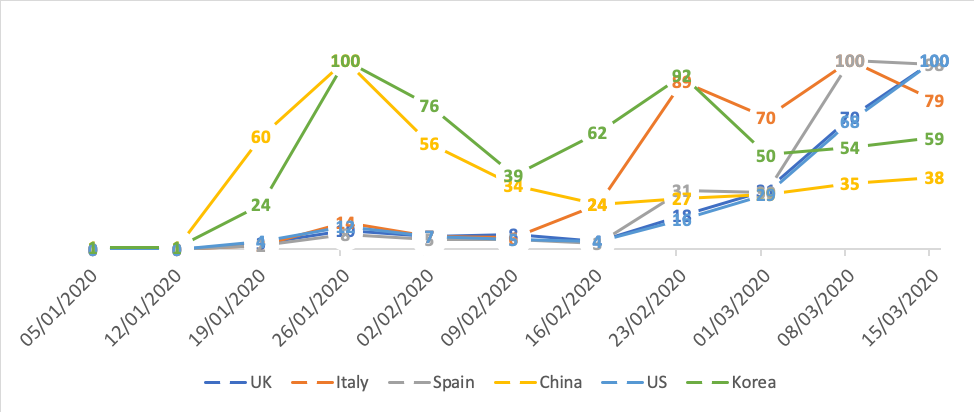
Similarly, the next figure suggests that most countries, except for China and Korea, did not pay much attention to the coronavirus until early February, when we saw a spike in Italy, and only after the second half of February there was an increase in attention in Spain, the UK and the US.
Google trends for ‘coronavirus’ in selected countries
One way of explaining how risk proximity affects people’s behavior is that behavioral reactions seem to depend quite heavily on how other people react as the crisis propagates, and on whether they modify their behavior in the face of risks.
What can we do?
Obviously, the provision of clear information plays a role in reducing the social formation of alarmist decisions. However, in planning preventative measures one needs to take into consideration that individuals only change their behaviors when they observe the risk in close vicinity and are extremely sensitive to what and how the media reports it, as well as reactions in their social environment. In pandemics such as the COVID-19, the speed of contagion is at a global level, which renders decisions based on risk proximity inefficient.
In facing global pandemics, one needs to beat the collective action problem (‘countries only care about risk when it’s already affecting them’) by increasing the surveillance of outbreaks, adopting global (and, at least European-wide) decisions that pre-empt delays in intervention, and more generally, overcoming the universal fact that individuals only adjust their behavior when the virus arrives at their doorstep.






























































































